My Wife’s Breast Cancer Story

Personal Disclaimer: I am writing this to paint a picture of my wife Sona’s battle with breast cancer. Many people have seen and spoken to Sona since this battle started in December of 2018 and are simply amazed at how she has rebounded from this merciless fight. So many people have asked what our strategy was and looking back, life with cancer was too complex and overwhelming to recount specific details. So I decided to sit down and write this story outlining what we did to fight this battle together. Please note that, of course, this should not be taken as advice on what to do as an individual treatment plan. I am not a medical doctor, and neither is Sona. Individual circumstances warrant different approaches. There is not a one-size-fits-all approach, and this is certainly not a “do what we did” article. What I do know is that cancer is a heavily armed monster that requires deep professional expertise in the medical field, which is beyond the scope of practice here at OC Fitness Coach. Cancer can be a very personal experience for many, but being in the health and wellness field, Sona and I felt that if readers could take something away from our experience to improve their own situation, then it was well worth sharing her story.
Personal Disclaimer: I am writing this to paint a picture of my wife Sona’s battle with breast cancer. Many people have seen and spoken to Sona since this battle started in December of 2018 and are simply amazed at how she has rebounded from this merciless fight. So many people have asked what our strategy was and looking back, life with cancer was too complex and overwhelming to recount specific details. So I decided to sit down and write this story outlining what we did to fight this battle together. Please note that, of course, this should not be taken as advice on what to do as an individual treatment plan. I am not a medical doctor, and neither is Sona. Individual circumstances warrant different approaches. There is not a one-size-fits-all approach, and this is certainly not a “do what we did” article. What I do know is that cancer is a heavily armed monster that requires deep professional expertise in the medical field, which is beyond the scope of practice here at OC Fitness Coach. Cancer can be a very personal experience for many, but being in the health and wellness field, Sona and I felt that if readers could take something away from our experience to improve their own situation, then it was well worth sharing her story.
How We Met
I met Sona shortly after I moved to California in the summer of 2009. She contacted me while looking for a personal trainer. I did not have many clients at the time. I was still renting space and training out of a small gym in Rancho Santa Margarita, Orange County. Back then, I juggled my passion of training the few clients I had during the day with being a security guard at The Montage Luxury Spa Resort in Laguna Beach at night. It was a way to get by and pay the bills while pursuing my dream of helping others live a healthy life. I was more than happy to take Sona on as a client.
Sona was born in San Diego to parents who immigrated from India. I remember her being so fun with a great sense of humor. She made me laugh ALL the time. She was successful and attractive. I’m not sure why she chose me, but I certainly didn’t ask any questions. After a month of training at the gym, we transitioned to in-home training. One night after training, Sona asked if I would like to stay for dinner. She was a great cook and learned from watching her dad in the kitchen at such a young age. One dinner led to another and we started hanging out more and more. Some of my favorite dishes she made were grilled tri-tip tacos, papaya salad, pork fried rice, mango salsa, grilled cheese sandwiches, sauteed scallops, pozole, homemade Persian, Korean and Indian food. She made healthy food taste great, which a lot of people have a hard time doing. Her cooking skills alone won me over, on top of all her other attributes. Sona’s talent for cooking and desire for a healthy lifestyle made us a great match, and at some point, I evolved from her trainer to her boyfriend. She was amusing to train, she was entertaining to hang out with and she was good at almost everything she did.
She was class valedictorian in high school, breezed through her undergraduate degree in the chemistry program at Syracuse University, then proceeded to graduate from a top-tier law school at UC Davis. Perfectly organized, she dotted her “i”s and crossed her “t”s. She was the first person to advise me that handshake deals do not pan out well in California. She was impossible to beat in any logical argument. Believe me, I tried, and for that reason, I told people the worst thing about her was that she was so smart. She was petite in stature, incredibly sweet and wore her heart on her sleeve. When you looked at her, she did not appear threatening or even physically powerful in any way; however, she packed a punch fueled by her intelligence and had the sharpest set of claws to unleash on rude or unfair people crossing her path. Anyone close to Sona knew this about her. She was intense when necessary, yet one of the most humble, caring wife’s and mother outside of the corporate world. The contrast was nothing I had ever seen before. Sona was the type of person who needed order in most areas of life or things would go haywire. She was obsessive-compulsive at times – perhaps that’s how she got to the top in her career, but we later wondered if these stressful tendencies may have led to some dysfunctions leading up to her cancer.

On April 20th, 2012 we got married in Newport Beach. Nine months and five days later, Sona gave birth to our first son Kale. Our second son Chance arrived in 2015. Life was good. If I would want to brag, I would say life was great.
Shortly after Chance was born, my business got busy, very quickly. Sona took on even more hours on top of her day job to help me scale and support my business: She helped with payroll, taxes, accounting, insurance, permitting, marketing, phone calls to potential clients… you name it, she did. She was a huge asset to my business, especially early on in the building years.
She was the mastermind in the shadows who lined up everything that paved the way for success to the matrix for OC Fitness Coach. She did more than just keep everything from falling apart, she helped me transform a “side job” and a dream into a legitimate business and a career. This was on top of her already stressful full-time job of writing and filing patents all day long as an attorney.
The Diagnosis – December 2018
In 2017, Sona was diagnosed with ulcerative colitis. Looking back, this should have been a sign for us to slow down, but instead we pushed harder, took on more projects, and continued to get swallowed up by the Orange County grind. I consider this a missed opportunity. Looking back, I personally believe that the stress, gut issues, and cancer were somehow all connected. Stress has been traditionally tied to declines in cognitive functions, gut health, and heart disease risk. However, some evidence also points to its possible impact on the growth of cancer.1
Then, in the fall of 2018, Sona discovered a movable breast cyst. The lump was somewhat new, and it appeared to change in size day by day: the cyst would appear to be smaller, then larger, then smaller again. It was confusing. We discussed going to the doctor prior to actually going, but work physically and mentally consumed us both and it was easy to lose focus on it. Of course, Sona had done regular annual physicals with no previous cause for concern. The cyst was soft, movable, and seemed to change daily, especially before and after her menstrual cycle. These all “appeared” to be telltale signs of a benign breast cyst.
Sona was also coming off a difficult summer, having lost her brother due to complications with his chemotherapy. Stress was high. It was an emotional time, and a busy year with her job as an attorney. She was also helping me manage an extremely busy year at OC Fitness Coach, not to mention the time commitment involved with our two young sons who had grown to be 5 and 3 years old at the time.
It was around mid-November that year in 2018, when the cyst seemed to really take on a new form. It was noticeably bigger than just weeks earlier, and we planned on getting it checked out after our Thanksgiving trip to Arizona. We began to get concerned, while fishing for reasons to convince ourselves to not be concerned. In the first week of December, we arrived at UCI Health’s Pacific Breast Care Center (PBC) in Costa Mesa. They performed an ultrasound, and the results seemed suspicious, so the radiologist decided to perform a same-day biopsy.
The doctor told us that he could usually spot malignancies versus benign tumors; but this one had him puzzled. The biopsy took 20 minutes to get a sample of the “cyst” that the medical team was investigating. Underneath the moveable tissue we were feeling, they found a mass measured at roughly 5 cm or 2 inches. This wasn’t the movable component we had been feeling the last few months. An immovable mass was underneath the cyst, almost as if it was hiding.
Five days later, after anxiously awaiting a phone call from the doctor, we still hadn’t heard back. Sona and I decided to call and inquire about the results. I didn’t want to make this phone call at home with our young boys’ present, so we left them with our nanny Rosa and drove away from our house, parking on a random street to make the call.
I called PBC, and over the phone the doctor confirmed that it was cancer. Ironically, this was two weeks after I had found out that my mother had also been diagnosed with breast cancer. A family friend and physician who worked at UCI Health sent us a detailed outline of the pathology report within the hour after discussing it with the radiologist:
The Pathology Report
-Left Breast IDC (Invasive Ductal Carcinoma)
-Metaplastic Squamous Cell Type
-Estrogen Receptor Positive
-Progesterone Receptor Negative
-Her2 Negative
-Ki67 (Aggression/Proliferation Rate) 30-40%
Sona was upset, reasonably so, but I felt a sense of relief, as if we finally had a starting point to work with. There was no more guessing. It was time to figure out how to tackle this beast who had snuck into our lives. I kept telling her that now that we knew what was going on, the planning could start. We did not know the entire scope of the disease, but we had some kind of direction.
The next step was MRI imaging, which was conducted the week following the diagnosis. It was mid-December, and at this point we wanted to get a clear picture of the mass, the size, and whether or not the tumor affected nearby lymph nodes. This was an intense procedure since the results could change the course of treatment, depending on if it was a local occurrence limited to breast tissue only, versus a regional occurrence including lymph nodes, or even a “distant” occurrence that had already metastasized to distant tissues and organs. Those who have ever had the displeasure of being inside an MRI machine know that it is not the most comforting setting. You are confined to a narrow space with loud noises during the entire procedure. And in addition to the tests that needed to be done, examining the scope of this potential deadly disease added even more stress.
Sona always wanted me to be with her in the imaging room, holding her hand, although the medical staff positioned her face-down. One of the most heart wrenching images that stuck in my mind from this whole experience was during her first MRI. Because of the deafening sounds of the MRI magnets racing through the metal tube, I could not hear Sona crying because the machine was so loud, but I could see her tears falling towards the floor as she was lying face-down. I felt like this cancer was bullying my wife and I couldn’t do anything about it. I wanted to physically fight the cancer many times, which sounds ridiculous, but this fight would not be physical, at least not for me. The best chance at knocking this out would be by both of us exhibiting calm, patience, level-headedness, relentless optimism, and undefeated focus. I never once became emotional throughout the entire experience because Sona’s emotions fed off mine. If I was focused, she was focused. If I was confident, she was confident. If I thought everything was going to be ok, then so would she. We would not allow emotions to control the planning, process or outcome.
Sona kept telling me that she wanted to “feel normal.” The last thing she wanted was for people to feel sorry for her and to be overly concerned. She did not want to be seen as the “sick person.” She was not about to have a switch in identity because of this diagnosis. She realized she was still a mother, a wife, sister, daughter and had a career she loved. She would do whatever she could to not let anything get in her path. She opted out of survivor groups and social support groups. We are not anti-religion by any means; however, she did not want those who knew about her cancer to “pray” for her. This made her feel only closer to death, or “ill and morbid” in her own words. She did not want to feel like she was dying. We decided not to disclose her condition to many people. We told my trainers at the gym, a couple of clients that were connected in the medical field, my sister, my dad, and a couple of our closest friends. We did not involve most family members, and told our boys that mom had a shoulder injury that required a lot of doctor appointments. It was not until late August of 2019 that Sona actually stopped wearing her wig around our boys, but we stuck with the original story. They knew nothing other than mom often wore a knit cap, took more naps, and had more doctors’ appointments.
The Cancer Spreads – December 2018-January 2019
Results from the mid-December MRI showed activity in the lymph nodes near the left armpit, so doctors conducted another biopsy to see if the cancer had moved from the original site. Within an hour we received a phone call that the two lymph nodes tested positive for cancer cells too. Obviously, we were hoping that this would not be the case.
The two positive lymph nodes warranted a PET/CT scan to see if the cancer had metastasized to other areas of the body. Our worst-case scenario would be a scan showing cancer in the distant regions such as vital internal organs. To put it mildly, a lot was riding on the results from this upcoming PET/CT scan. It was stressful, but once again, we needed to remain focused on solutions.
We needed to wait 2-3 weeks between the MRI and the PET/CT scan because of the holidays. Since this was all happening around Christmas, we were juggling the medical stress and doctor appointments, while trying to stay positive and plan a festive Christmas season with our boys. We went to the Newport Beach boat parade, put up Christmas lights in our home, arranged Christmas presents for the boys, and planned Christmas Eve and Christmas Day parties with snacks, games, and movies. We wanted to give our boys as cheerful of a Christmas as any other year, while keeping almost everyone in the dark about what Sona and I were going through. Despite all the craziness and chaos and the anticipation of what was to come, our boys had a great Christmas and enjoyed a lot of good quality time with their mother.
In the weeks prior to starting treatment, I was trying to pinpoint why this happened to her. At work, I quietly sat at my desk between client appointments, staring at the wall, trying to figure this all out. As a trainer, health coach and nutritionist, I was well-aware that no one is bulletproof, and cancer can happen to anyone. But her diagnosis took me by surprise, considering her age, her lifestyle, her body weight, her activity level, and her diet. There was also no genetic factor or family history of breast cancer.
As early as that first night after the diagnosis, my sister Katie and I were researching everything about breast cancer, from how conventional treatment worked, to alternative and natural treatments, nutrition therapies and other lifestyle modifications that we could present to Sona to put up the strongest fight. She and I quickly realized how incredibly complex cancer is. Just when we thought we had the scope of cancer in our crosshairs, we would become even more confused. My sister and I would volley scientific journal articles and medical websites back and forth after finding them online, sometimes late into the night when Sona was already sleeping. One article would say something, and the next would say the opposite. We read a lot of information and experienced information overload. However, our mission was to squash cancer from every angle, close off all entries to Sona’s body, hit this thing head on with intensity, and possibly try to add somewhat controversial therapies to ride along side with the conventional therapy that was ahead. Additionally, we planned to “stay over the target forever.” Yes, even if we managed to get rid of the cancer, (which I was more than confident we would) it was important to do everything we could to make sure it would not return.
The night before the PET/CT Scan Sona and I re-watched the hockey movie “Miracle.” Not necessarily because we were hoping for a miracle, but because I loved watching the Team USA hockey coach’s decision-making skills. Coach Herb Brooks reminded me of my days as a paratrooper in the 82nd Airborne Division in the Army. Our Army commanders were rarely ever “liked” however they got shit done, and that was all that mattered here. We needed to get shit done regardless of worrying about who we pleased, who we upset, who agreed with our strategy and who did not. I was appointed overnight by Sona (the day of diagnosis) to drive all the decision making for our battle plan. I had always helped people with their health issues such as weight loss, diabetes, arthritis, heart disease and multiple sclerosis, but cancer treatment was all new to me. I was confident and more than determined to bring everything I could to the table.
The next morning was a cold Friday morning in January. We drove to UCI in Orange for the PET/CT scan to see if the cancer had metastasized to distant vital organs. For over an hour, I sat and waited as Sona got prepped for the procedure in the back with a technician. They called me in as the procedure began, and I sat with her in the imaging room. I remember trying to analyze the techs’ faces and gestures as they were performing the scan, staring at real time imaging on the screens in front of them. There was little else for me to do during this incredibly important procedure. As we finished up the imaging, we were once again told, “The doctor will contact you with your results.” We drove back home and waited. And waited. The procedure was in the morning. So as the 12:00 o’clock hour came and went, I was over-analyzing the wait. Maybe they were at lunch? Maybe they were planning on how to break the news/results to us. Two hours later, as I was texting with my sister, the phone rang from UCI Health. One of our favorite doctors throughout the whole process was excited to tell us that the PET/CT scan did not show any signs of distant cancer. The cancer had not spread further to other areas of her body. This was the news that we were hoping for. It gave us a much-needed break, a spark of hope, and a morale boost. It was the final piece of the map before we could put our battle plan into action. The question now, was to decide which treatment plan we wanted to proceed with.
The Battle Plan For Treatment
Our treatment plan options were overwhelming. Many outsiders looking in, bloggers, and holistic practitioners (which I would consider myself to be) advised against the dreaded conventional treatment. Chemotherapy, radiation, and medication did not sound appealing to us either. However, considering the size, lymph nodes, hormonal profile and the Her2 status, we felt that we wanted to combine both conventional and additional therapies, and that this approach would yield the highest chances of success.
Prior to making this decision, I read several journal articles and books on how to beat cancer through nutritional therapies and was introduced to the concept of functional medicine. Although we were fortunate enough to have an amazing medical team of renowned professionals at UCI Health during the entire process, there were never any conversations as to how or why this happened to Sona, and – more importantly – how to make sure it does not come back. The conventional medicine approach (i.e., chemo, radiation, medication) were all aimed at cutting off the “dead leaves on the tree,” which was important to stabilize the disease, but to get to the root of why this happened we needed to dig into the roots of the tree, and to ensure this would never come back.
During this entire time, I was navigating the options with my sister, weighing the pros and cons, the risks and details of both options. Some people in the “circle” – those who knew what was going on, advised against chemo saying it was a very bad choice. This was frustrating because, despite being in our trusted inner circle, they remained outsiders looking in. Of course, chemo was toxic, potentially lethal, and poisonous to the body, as it has to kill cancer cells inside a living human being. And Sona probably knew more than anyone because her brother had just passed away months prior. However, I felt that I did not have enough knowledge or confidence about natural treatments to experiment with them and to trust them alone without conventional intervention.
It was nauseating to look at all the options on paper, but we needed to make a decision. I was getting very irritated with people telling me how horrible chemo was, when they were not the ones trying to fight the disease. It is always easy to be a back-seat driver in this situation. After reading through what seemed like a mountain of articles on the subject matter, I felt like I understood the negative effects of chemo and radiation. So did Sona. We knew the risks. I even watched “The Truth about Cancer” TV series. I was getting really angry with unsolicited advice but learned to not get overly worked up by it. I needed to mute certain things I would hear or read on websites discussing phony supplements, false diets, hokey pokey herbs, and ancient medicinal practices. It was all so overwhelming. That is not to say that some of these approaches may or may not work, but when you have hundreds of strategies that all supposedly kill cancer, life gets overwhelming pretty fast. Attempts to weed out fact from fiction was a daily task that took a lot of time. All we could do was research, make our best guess, and welcome the medical professionals’ expert opinions on the matter. After all, we were thrown into the position of fighting this beast in a short amount of time.
Sona elected me to be in charge of the process and drive the decision-making. I would brainstorm with her, but at the end of the day, she didn’t want to focus on it because it would destroy her mentally. We decided to fight her cancer with conventional treatments but not rely on that alone, and then build her body back up after the damage of the chemo killing off her cancer was done. We knew that chemo was going to present its own challenges but were confident that we could rebuild her back up through advanced lifestyle and mindset therapies during and after the whole process played out. Essentially, we wanted to take care of the roots of this disease after the medical professionals did their part.
For starters, we wanted to gain an advantage on chemo. We both felt that our oncologist at UCI Health, who I won’t name, rushed our conversations and did not explain the treatment plan well enough. He rubbed us the wrong way throughout the process, but we had to learn to work with him, because at the end of the day, he still knew what he was doing and that’s all that mattered to us. There was confusion very early on about her case. He kept telling us that her tumor was expressing itself more as triple negative breast cancer, and that treatment might be limited. For weeks, I did a lot of reading on what triple negative breast cancer was, and why in certain cases it can be hard to treat. It was not until weeks later that it was explained to us that this was indeed a hormone-sensitive breast cancer profile. The advice of our first oncologist, who gave us the impression that her cancer would be hard to treat, was that we follow a “watch and wait” strategy. Considering the implications of chemo, this did not sit well with us. I remember thinking, “Are we going to go through all this chemotherapy and just “hope” it works?”
Functional Profiling and Cancer Cell Response
After doing more reading, I came across a doctor in Long Beach who conducted personalized cancer cell testing, which exposes your living cancer cells to different chemo agents. He would send us a detailed report showing which agents were used and if they were effective in killing her specific cancer cells. We brought this up to the UCI Health oncologist and he didn’t show much interest, claiming that this type of personalized testing still produced mixed research results and was in its infancy. Fair enough, I guess. But in spite of that, we drove to Long Beach on a rainy day in January, completed another biopsy, and within a few days we had the test results of the assays. This laid out specific agents and labeled them as resistant, sensitive, or active. Based on the test results we knew exactly which agents worked and those that did not.
How Nutrition May Support Cancer Treatment: Ketogenic Metabolic Therapy
I read the nutrition plan he gave us put out by the American Cancer Society (one section suggested ice cream, milkshakes, candy, and sugary drinks) and was very resistant to taking their directive and applying it to Sona’s plan. I kept in mind that I was not a medical doctor, oncologist, or registered dietician, but these recommendations just did not sound right to me at all.
I reminded myself that I was a rookie at this cancer diet, but I kept reading. One article or book would lead me down one path, which then put me on another path . Eventually I started reading about meal timing, time restricted eating, phytochemicals and their potential cancer-fighting effects, foods such as cruciferous vegetables, garlic, green tea, flaxseed, onions, leeks, and shallots, which led me to look into the ketogenic diet to fight cancer.
There have been hopeful arguments that have suggested cancer originates from damage to the mitochondria and depends on the availability of fermentable fuels for tumor cell growth and survival.2 In the 1920’s, prominent German biochemist Otto Warburg hypothesized that cancer cells take up much higher amounts of glucose than other cells and surrounding tissue. He concluded that cancer cells could be “killed off” by starving the cells of glucose and oxygen.3
There is a great deal of confusion and uncertainty when it comes to dietary practices for people going through cancer. The Ketogenic diet has been used since the 1920s for the treatment of epilepsy and is generally comprised of high fat, moderate to low protein and very low carbohydrates. More dietary carbohydrates result in more glucose; therefore, the plan was to start a keto diet with the premise being to fully eliminate sugars and minimize carbohydrates, especially refined carbohydrates overall. Recent research has suggested that ketogenic therapy could have a tumor growth limiting effect on cancer and cancer cells, while protecting healthy cells from the damaging effects of chemotherapy and radiation while lowering inflammation.4,5,6 Although the evidence was encouraging yet not necessarily conclusive, I still was confident enough to add the ketogenic diet to Sona’s plan. Perhaps in the coming years more research on this diet can shed light on this strategy to help others effected by cancer.
In addition to keto, we added intermittent fasting. Simply stated, fasting is selecting specific times when one can eat, and other times when no food is to be consumed. Our train of thought with this additional therapy was that fasting would lower insulin levels, improve insulin sensitivity, and lower glucose which we would hope would result in lower IGF-1 (insulin like growth factor) which many cancers rely on for proliferation. IGF-1 also suppresses apoptosis (the cells ability to kill themselves – a protective mechanism to eliminate dysfunctional cells) and promotes progression, angiogenesis, and metastatic activities in many cancers.7
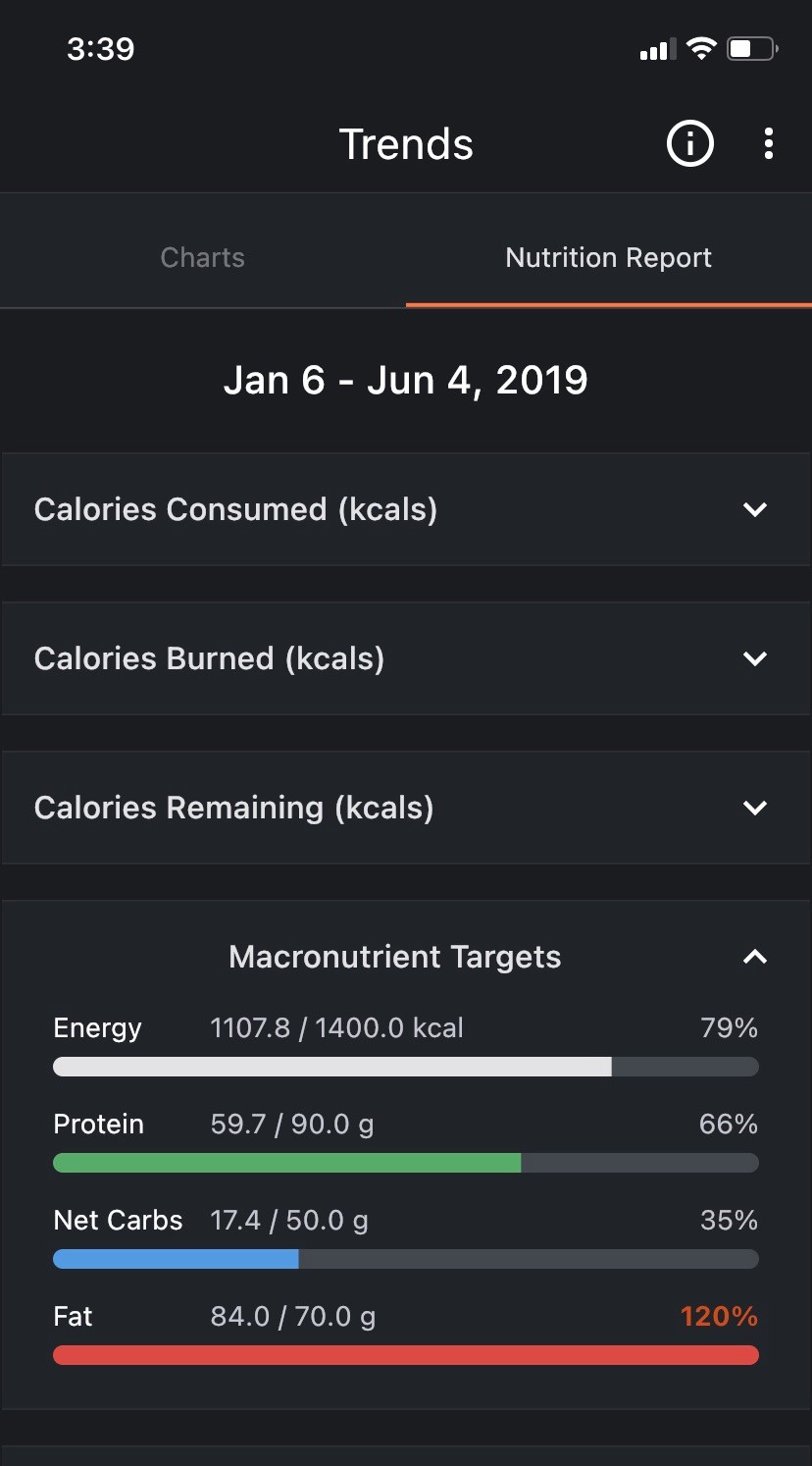
Sona was very persistent with the keto diet, never wavering once during the 6-months of chemo. Although the boys were too young to notice, she did not have one bite of cake on Kale and Chance’s birthdays, which brough tears to her eyes. She averaged 1,108 calories, 17.4 net carbs, 59.7 grams of protein and 84 grams of fat per day (see screenshot). The idea behind keto was to “starve” the cancer of glucose through limited carbohydrates while utilizing ketones as the supplier of energy to the healthy cells. One of the potential hurdles with this diet was malnutrition, so we focused on consumption of only nutrient dense foods high in vitamins, minerals, essential amino acids and essential fatty acids. Her diet was comprised of wild-caught salmon, macadamia nuts, garlic, avocados, cruciferous vegetables, MCT oil, chia and hemp seeds, and on occasion grass-fed beef. Along with avoiding all sugar and most carbohydrates, she avoided processed fats and proteins (soybean oil, vegetable oils, non-organic animal products, high fat keto desserts). She would not consume any of the stereotypical foods often associated with keto, such as bacon-wrapped butter, fried cream cheese sticks, heavy cream, keto ice cream, or greasy protein style burgers from In-N-Out.
Chemotherapy – February 2019
In early February, a week or two after our Long Beach visit, Sona began chemotherapy every Wednesday at the Pacific Breast Care Center in Costa Mesa. These treatments lasted through June, and although we did have a nice view of the Pacific Ocean, the place was incredibly depressing. In the five months of us being there, we must have seen only two or three other patients younger than Sona. All the nurses knew us by name. I would drive her and take my laptop to do schoolwork, as I was just six months away from finishing my master’s degree in Nutrition. She would also bring her laptop to work, but after a while we put aside our work and just used that time as time for us. There was a coffee maker, a snack drawer and a refrigerator full of water. It was not long before we looked forward to Wednesdays as our date day at the treatment center. A strange place for a date, but it was time for just us, away from everyone, including the kids and work. It took us a few sessions to get used to the hospital environment and its surroundings, but we both eventually enjoyed Wednesdays in a strange way. It was fun.
I would always try and bring humor to the situation during chemo and throughout the entire experience. This was absolutely crucial during the entire process and I can’t stress that enough. We would laugh as usual, make jokes, and pick on each other just as we always did. Sona wanted things to be normal, and I did my best to continue making “normal” happen. When she started losing her hair, I joked that she looked like Shakespeare. Most days she would wear a bandana around our boys and I teased her by saying I felt like I was married to NFL Hall-of-Famer Deion “Prime Time” Sanders. When her eyelashes fell out, she wore fake eyelashes and I told her that the fake ones she wore made me feel like I was hallucinating on mushrooms when I looked at her. The things that others would expect her to be sensitive about, I teased her about, all in an attempt to make her feel normal. This is not meant to be insensitive to others that have had friends and family members go through this. My intent the entire time was to make her feel normal and to make her laugh, like I always had in the past, and it worked for us. It was incredible how strong she stayed during the whole chemo process. My dad told me something early on during this time that really resonated with me. He said that you get married to be there for your spouse in times like this. Many people only envision the good times in marriage such as dining out, wild nights in Vegas, or vacationing in Europe. That conversation stuck with me and helped me stay grounded throughout the process.
In March, we had a bit of a worry after meeting with the breast surgeon. The “cyst” that had been present for weeks prior to diagnosis had not changed much or shrunk. It was hard to determine if the chemo and the diet we decided on were actually working. We also met with the radiologist and oncologist that morning. They were puzzled and decided on another MRI and told us that they would opt for surgery if “chemo wasn’t effective.” For the next three hours we waited for an MRI after lunch to figure this out. Sona was having a very difficult time with the anticipation building up to this MRI. The words of the oncologist sat with her, and she was thinking that the chemo was not as effective as intended. After the scan, we went back to the waiting room and waited. The radiologist came out with a smile 20 minutes later and told us the tumor had shrunk over 50% of its original size. Meaning, despite the cyst still being there, the cancer was shrinking rapidly, and it gave both the medical team as well as me reassurance with the treatment plan, nutrition, and lifestyle modifications that we made.
For our anniversary in April, Sona and I dined at our favorite restaurant, Mastro’s Ocean Club in Newport Beach, and in May, before a heavy dose of the “Red Devil” chemo protocol, we went to Lake Havasu for a four-day weekend. We still did our best to enjoy life and our family in spite of the difficult path we were traveling.
Sona’s strength, determination, and care for our boys and myself during this time was amazing. On the days of chemo, she would often go to the store and make sure we had enough food to make dinner for the boys and me. When I would tell her to go rest in bed, she would tell me she just wanted life to feel normal.
One day in May, I had a presentation on senior fitness and nutrition scheduled at an assisted living facility. I had scheduled this presentation months in advance. At the last minute, I had an opportunity for an unplanned consultation with a very good potential client who had limited time. The day before my presentation, while we were in chemo, Sona drafted a slide deck and PowerPoint presentation for her to present my business to this group of seniors at their facility.
The following day she stood in front of everyone at the senior facility, explaining OC Fitness Coach. She knocked it out of the park, however this came as no surprise to me. Most people thought she was a healthy, in-shape trainer and nutritionist, not the wife of the business owner who was filling in due to a last-minute client meeting, and certainly not someone who was attached to an IV drip with chemotherapy the day prior. It was incredible how much strength she had throughout the process. I could not believe that she kept pressing forward as if nothing had happened and would only occasionally be thrown off track emotionally.

Of course, there were days when she had less energy, required more sleep, and battled nausea. But she would not show it. Every Sunday morning, I would throw Kale and Chance in the truck, let Sona rest, and drive down to my studio at Lake Mission Viejo, and teach them Brazilian jiu jitsu and boxing. Upon returning Sona would always have blueberry pancakes ready for the boys. She never missed a weekend. She told herself she was not going to let this battle affect her job or her relationship with her kids and her husband.
With her wig placed gracefully on her head, she put on her poker face and had everyone fooled, despite the toxicity of chemo. She never had a victim mentality or got into “why me” discussions. Many days she would feel worn out, but still volunteered in our kid’s school classrooms, drove them to birthday parties, planned weekend activities, and took care of everything a husband would need or want in a marriage under normal circumstances. Often, she would not allow herself to rest, resulting in protests from me. Sona was such an inspiration to me and the true hero of this story. She never allowed the events that were unfolding to take her motherhood and connection away from our boys. Kale and Chance knew nothing, so they would have their age-appropriate meltdowns, struggles and frustrations, but I kept telling them how fortunate they were to have their mother.
Sona also supplemented with various remedies such as bone broth, trace minerals, medicinal mushrooms, green tea phytosome with EGCG, turmeric/curcumin, vitamin D, and CBD/THC gummies. None of this was at the advice of the oncologist. We had no supplemental suggestions from the medical team. This was all based on our readings. I cannot say with 100% certainty that all of these supplements made a difference, however, we decided to do this based on promising evidence from our readings and limited background in cancer treatment protocols.
She would do intermittent fasting 24-hours prior to chemo and 24-hours after chemo for a total of 48 straight hours, and only consume water with electrolytes. On top of this, she would do a 16-hour daily fast most days of the week, only eating between the hours of 12:00pm and 8:00pm. Some days she would push this to a 6 or 4-hour eating window. Although preclinical data in nature, a study from The University of Texas Southwest Medical Center showed mice who completed an intermittent fasting protocol had fewer cancer cells after seven weeks versus the mice that were well fed and did not fast.8
We notified the nurses as to what she was doing, and they could not believe it, as if they had never witnessed any other patients doing this. I tried to find reasons why this was not a good idea but nothing was convincing us not to try it considering Sona’s individual circumstances. Some of the nurses saw this as risky. In contrast to this, the cancer center always had sweet treats out for the cancer patients, which based on all the reading I had done, did not seem like a good idea. However, I was never in that role as a cancer patient and I was not the doctor. Many more things go into cancer patient nutrition such as comfort, emotions, or nausea. It is not always about making the healthiest choice for chemo patients, and I respected that.
Although we were very happy with the overall experience with our medical team throughout chemo, it was our self-imposed education on cancer that stressed the importance of nutrition, stress management, sleep optimization, exercise, and toxin avoidance. On the rare occasion that we brought up some of these holistic therapies to our oncologist, they were quickly dismissed as having no scientific evidence despite the fact that we had read of stories suggesting otherwise.
Sona’s chemotherapy finished in mid-June 2019. The doctors wanted a month off before surgery to heal. We kept this day (Wednesdays) reserved for “date morning” and would go out to breakfast while I had other trainers cover for me at work, until I returned for afternoon training sessions. These breakfast dates were frequently in Laguna Beach and we would often go walk around and stare at the ocean at The Montage which brought back memories of when I was working there when Sona and I first met.

As far as her diet was concerned, we tactically boosted her carbohydrates slightly and added a bit more protein before surgery, due to a decrease in lean body tissue throughout the first few months. We were aiming to put some mass on her before surgery. We wanted to prime her body and put her in the highest state of wellness that was possible for her at that time, like we did before chemotherapy started.
The weight loss had nothing to do with cachexia or muscle wasting commonly seen in many people in various chronic disease states. It was due to the fact that two days a week she would not consume any food, and a diet which consisted of not even 20 grams of net carbs a day for six months, with limited resistance training. Weight loss can pose a potential risk in certain individuals.9 However, she was weighed weekly, with weekly CBC panels and other blood markers for the oncologist to review, and they never addressed or showed any concerns.
Surgery – July 2019
Our alarm went off at 4am on July 15, as we got up early for surgery and drove back to UCI in Orange for our 5am check-in. This was the same place we went for the PET/CT scan in January. Surgery would be at 8am. Sona was nervous and had a bit of a meltdown before we left the house. She did not want to go; but I stuck to my tried-and-true “just make her laugh” strategy. Thankfully my jokes, often inappropriate in nature, still made her laugh despite the long day ahead.
I sat in the waiting room from 7am-4pm focusing on my schoolwork. At one point, one of my fitness clients, who was a breast cancer survivor as well, stopped in for an hour and we talked about everything; Her breast cancer progress, Sona, my business and Anaheim Ducks hockey. Additionally, our UCI physician friend brought me lunch from the cafeteria. It was a long day in the waiting room, and not the most pleasant of places.
Sona needed her breast tissue and multiple lymph nodes removed. At around 10:30am, the surgeon came out and gave me a visual thumbs up as she was approaching from the other side of a large room. I went into a smaller side room with the surgeon, and she told me that the remaining tumor had been removed with great margins, and that she had to take out more lymph nodes than originally planned. However, she reassured me that the surgery went well. Sona was still in surgery for another 4-5 hours for reconstruction. I was following the color-coded surgery board with our patient ID and viewed the status often to see if it was listed as pre-op, in-surgery, post-surgery, or recovery.
At 3:45pm the color changed to post-surgery. I waited another hour or so until the nurse came to get me to bring me back to Sona in recovery. She was still very incoherent from anesthesia, and we were in the recovery room for another 2 hours. At 6:30pm, we were able to get to a room where Sona’s boss (whose wife is the UCI physician previously mentioned) came to visit post-surgery. Sona FaceTimed with our boys around this time and the story was that she was at a business meeting in San Francisco. Shortly after, I raced back home (about 35 minutes away) to be with Kale and Chance for an hour. I spent some time outside playing soccer with them, gave them a bath, and read them a book before putting them to bed. I rushed back to UCI Health, and we ended up spending three nights at the hospital while our nanny stayed with the boys. I remember every morning during our stay at UCI the doctor would come in with about 6-7 med school students. They would all be in their white coats and as I saw them in the distance I would signal to Sona: “The White Coats are coming! The White Coats are coming!” in a Paul Revere kind of tone.
As the following weeks went by, things were moving along nicely, however Sona had very little muscle mass, limited range of motion, and was in full recovery mode post-surgery. The surgeon gave her basic exercises for rehab purposes. After about 10-14 days we started the rehabilitation process with exercise.
Rehab Training-Post-Surgery – August 2019
In August, Sona came back to train with me initially at our Mission Viejo studio. We would do stretches and range-of-motion exercises with ghost weights (meaning no weights whatsoever, just the movements involved in the process). While it looked foolish, it was important to get her body moving, re-establish movement patterns, regain muscle and to get the lymphatic system up and running again.

There is a high risk for lymphedema that often occurs after cancer surgery when lymph nodes are removed. The lymphatic system is part of the immune system and a group of vessels throughout the body that filter waste products, bacteria, and viruses away from vital areas of the body. Disruption in this system can lead to an increase in infections and a decrease in immunity. Our game plan was a combination of movement exercise with therapeutic massages to prevent this from happening.
Radiation – September 2019
Now that the tumor was removed, I was as confident as ever that I would be able to build my wife back up with nutrition and exercise, returning her strength, endurance, muscle mass and overall bodily health. Slowly she was gaining strength back and general confidence. A few weeks post-surgery, in early September, Sona started the next phase; radiation in Laguna Hills in an effort to kill off any potential free-floating cells in the area, although the surgeon and oncologist were more than optimistic that the cancer had all been removed. She had a few weeks of radiation, Monday through Friday daily for 5-10 minutes. There was minimal burning, she temporarily avoided the sun, used natural healing oils and cream, and consumed nutrients specific to helping with the negative effects of radiation.
I remember the first day when Sona was getting treatment, an older lady was there for her first day as well. She asked about me, and I told her about Sona, but did not mention what we went through the previous few months. She was strong, graceful and you could tell she valued life. It’s unfortunate when you see healthy people who are not going through any health issues acting spoiled, entitled and anything but graceful. I have much respect for those who have gone through this personally, or who have had family members go through this or other major medical conditions. Too many people have fought this battle or have seen a family member go through this. And whether one perishes from the disease or battles through it, everyone who has fought cancer is an extraordinarily tough fighter. Just like Sona has inspired me, cancer patients have a gift of inspiring others to march on through the darkest of times and value life and what you have. These people have a tremendous amount of strength that many people could never fathom to understand. Unfortunately, not all cancer stories have a happy end to them, as some people are not able to defeat their cancer, but that does not, and will never take away from their strength.

“Hey Everybody! I’m Ok!” – October 2019
At some point during the radiation treatment, Sona told one of the technicians with whom she had became friends with, that she would wear a Hooter’s outfit in support of breasts and breast cancer on her last day of treatment. She wanted to convince herself and the world that despite the swords and daggers thrown at her all year with conventional medicine, she was ok. At this point, everyone knew that she had gone through cancer treatment, but people didn’t have a visual image of her. I got the sense from some of the conversations I had, that people assumed she was in bed all day, unable to move or feed herself.
She wanted to let the world know that she was standing strong. She did not look like she had just finished extensive chemotherapy, surgery and radiation treatment. She looked more than healthy, and she wanted everyone to see this.
Building Her Back Up – December 2019
At this point, we ramped up the heat with positive lifestyle habits. We transitioned to more intense workouts to build muscle mass while keeping body fat low. From a goal’s perspective, we wanted to keep blood sugar from elevating, maintain a low body fat percentage to manage estrogen levels, build lean body mass, and re-introduce more carbohydrates to promote optimal thyroid health while still maintaining a low glycemic diet.
Sona began medication with minimal side effects, minus some mood swings. From the end of 2019 until today, she has been working out with my coaches Jerome, Codie and Tihana, while I focused on her nutrient-dense nutrition and lifestyle therapies. We bought a high-quality, low-EMF, full spectrum infrared sauna for our backyard along with a red light therapy unit which uses photobiomodulation. We have placed a huge emphasis on sunshine and vitamin D, B-complex vitamins, stress management, sleep quality and quantity, and overall joy in life. It is a very fair statement to say she is in great shape at this point. Standing at 5’0 and 107 pounds, she has dominated the weightlifting game, is physically stronger than ever, has upped her cardiovascular endurance, increased her flexibility, and can still kick ass as a mother, an executive and a wife.
The process was not all lollipops and roses. Those who have been through this probably know exactly what I am talking about. But despite the arguments, disagreements, and frustrations we had along the way, I am unbelievably proud of how Sona and I have handled this battle as a team. We will remain offensive in our approach. There have been challenges along the way, and they will continue to be there because this is a constant effort to ensure the cancer does not come back. We will not become complacent and will always be ready for whatever comes at us. Sona has recently had her last MRI scan showing everything is clear, and she is in a good place mentally.
We’ve chosen to rely not only on the typical standard of care, but instead seek out additional lifestyle therapies to optimize the body through a functional medicine lens. Our mission, I believe, has been amazingly successful. She has since opened up about her experience and has helped other people with cancer navigate through the process.
Whether someone is trying to avoid cancer, heart disease, mental impairment, or psychological issues, everyone can agree that too much stress is bad. It is all too often, especially with executives and others in Orange County and elsewhere, that I see people overworked, overstressed, overweight, and overmedicated, while being under-happy, malnourished, and playing “catch up” with their health. I often say that people overlook the foundational components of health while focusing on the smaller esoteric things (i.e., the best ab exercises, best treadmill brand, random juice diets, best exercise for fat loss). Exercise and nutrition are not the only important things to consider when it comes to your health. Be proactive with your health and your treatment plan. Read, research, talk to others, and discuss all available options with your doctors and health practitioners so you can determine the best plan of action when you are battling a disease or condition. Our continuous mission has been successful because of the combination of a highly skilled medical team and additional lifestyle therapies.
TO BE CONTINUED…
Dan Tatro-M.S., CSCS (CEO/Owner OC Fitness Coach)
REFERENCES
1. Bellastella, A. Stress-induced epinephrine enhances lactate dehydrogenase A and promotes breast cancer stem-like cells. Faculty Opinions. 2019; 129(3): 1030-1046. https://doi.org/10.1172/JCI121685
2. Seyfried T N, Yu G, Maroon J C, D’Agostino D P. Press-pulse: A novel therapeutic strategy for the metabolic management of cancer. Nutrition and Metabolism. 2017; 14: 19. https://doi.org/10.1186/s12986-017-0178-2
3. Liberti M V, Locasale J W. The Warburg effect: How does it benefit cancer cells? Trends in Biochemical Sciences. 2016; 41(3): 211-218. doi:10.1016/j.tibs.2015.12.001
4. Klement R J. Fasting, fats, and physics: Combining ketogenic and radiation therapy against cancer. Complementary Medicine Research. 2017; 25(2): 102-113. doi:10.1159/000484045
5. Klement R J. The influence of ketogenic therapy on the 5 R’s of radiobiology. International Journal of Radiation Biology. 2017; 95(4): 394-407. doi:10.1080/09553002.2017.1380330
6. Youm Y, Nguyen K Y, Grant R W, Goldberg E L, Bodogai M, Kim D, .Dixit V D. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nature Medicine. 2015; 21(3): 263-269. doi:10.1038/nm.3804
7. Brahmkhatri V P, Prasanna C, Atreya H S. Insulin-like growth factor system in cancer: Novel targeted therapies. BioMed Research International. 2015: 1-24. doi:10.1155/2015/538019
8. Lu Z, Xie J, Wu G, Shen J, Collins R, Chen W, Zhang C C. Fasting selectively blocks development of acute lymphoblastic leukemia via leptin-receptor upregulation. Nature Medicine. 2016; 23(1): 79-90. doi:10.1038/nm.4252






Comments are closed here.